Substitute Blood — A Failure Of Clinical Ethics
Life is fragile at best. At worst it is undervalued. Prolonging it and maintaining its quality is something most doctors have at least thought about.
Me — I was brought up by family values as well as institutional values to venerate the academic system as a seeker of truth, guardian of highest ethics.
I thought that the institutions that regulated clinical research, whether they were academic or not, were at least trying to be ethical in the face of mounting economic pressures from those who develop substances to be used for the human body, to prolong and maintain life. Some people still believe in this.
Some people, even some I can call “friend,” consider me a failed academic, someone who could have contributed more to society had she written more papers that somebody thought were good enough to publish in medical journals.
All of the above is unadulterated lies and total BS that has kept many competent minds devoting their lives to ideals that are later sold to the highest bidder.
I don’t think I have any lingering doubts that my running from academics, yelling and screaming, was the best decision I ever made.
The story of Polyheme – developed as a synthetic substitute for human blood — is perhaps the worst example of human rights having been sold down the river for development of something of serious danger (if you believe the publically published academic results) and at best, unproven help (are they really keeping this kind of secrets from us so the company developing this junk can make money?) to either prolonging or maintaining life.
The story is complicated, but basically, here it is.
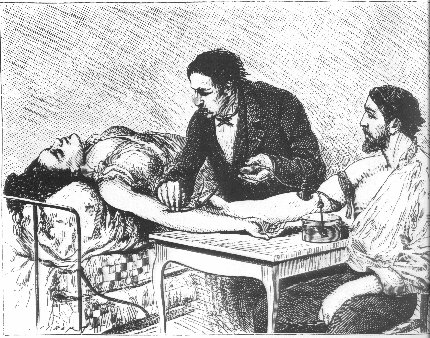
1. When people have serious accidents, they lose blood and the lack of circulating blood that brings oxygen to the tissues can — and does — kill people wholesale. The current thing for the paramedic types in the field to do, who don’t have time to cross match blood, is to use saltwater solution as a substitute for blood. Doesn’t do the trick for long, but at least it can maintain life temporarily. Of course, you have to keep pumping it in for a while as folks quickly pee it out, but at least it keeps the body alive. There have been various attempts to add stuff (crystalloid) that can carry oxygen and last longer for the medics out in the field. These substitutes are not, as far as I can figure, a dramatic amount of help either. Usually, once someone makes it to the hospital, they “type” the victim’s blood and people get the real stuff — or some part thereof. Some victims do well, some do not, and there are lots of factors you cannot measure since every human body is so wildly different and it is hard — if not impossible — if not a moral and ethical problem — to experiment with dying people.
It is interesting to note that there has absolutely never been any research I can find to prove that blood transfusion prolongs survival after severe accident. Blood types were discovered in 1909 and medicine has used this technology ever since. I am pretty sure it has saved lives. I guess we still do it out of some kind of magical thinking or belief or habit or tradition. This is why medicine is not and maybe should not quite be considered an exact science.
2. The argument in favor of the development of Polyheme sounds good ; so good, that Northfield labs bet the farm — literally, bet the company on its success. Teency-tiny hemoglobin molecules link together in groups of four and carry all the oxygen those of us who walk about in perfect health need. They are found on red blood cells which break down and go out of the circulation in 20 days. So the idea was, if hemoglobin molecules could be “polymerized” — that is, a bunch of them linked together — they may be both operative in oxygen carriers AND last longer since they would not seep out of blood vessels or break down or anything like that. A lovely idea.
3. When conducting a clinical trial – experimenting on humans with something that hasn’t been scientifically proven or government-approved yet – the sponsors are supposed to get an informed consent from the patient. This means that the patient is told everything that is going to happen to them, what results are expected, and what things can possibly go wrong. The patient must be aware of all the risks and be competent to agree in writing to undergo the testing, and this is all monitored by supposedly neutral parties (Institutional Review Boards – IRB) who have the welfare of the patients topmost in their priorities. And of course, all this must be reported to the FDA, who can – in theory –- step in and pull the test if anything looks doubtful.
The complication with a test concerning blood substitutes is that frequently the people who need this product are unconscious. So the informed consent is impossible.
The FDA has attempted to come to the rescue, as they have done this before for emergency protocols. If it seems that the greater good for the public – or all humanity – can be advanced, some exceptions can be made (by people we can only hope are competent to make such decisions).
Agencies similar to our FDA have resisted expedited review in other countries. And there are numerous times that the FDA “fast-track” has resulted in dangerous drugs being given approval to go on the market – only to be later removed because of adverse effects. Although the FDA has done this sort of expedited no-informed-consent sort of thing before, it had never been done on a blood substitute product.
I recall something from long before I became a physician. I worked as the lowly receptionist at the front desk in a highly respected emergency room. One of my duties was to plumb the pockets of unconscious trauma victims for identifying data — insurance cards, and the like. Remember, I was only 18, still a college undergraduate and everyone I told I would be a doctor laughed at me in disbelief.
Sometimes people came in who really desperately needed emergency procedures, really life-threatening. They were out cold and we could not contact a next-of-kin. We had to get someone with more juice than moi — a lowly receptionist with doctorhood aspirations – to make a critical decision. Usually this would be a senior administrator on-call who was either on site or home sleeping. I would tell the story and secure either the administrator’s signature – if present — or I documented that I had called the guy at home.
This person placed his career and possibly the liability for the entire hospital on the line, and was expected to act with the highest ethics. This representative gave informed consent for the unconscious patient as a “hospital surrogate” and I took no small risk by documenting verbal consents carefully. A weasely person could easily back out later on and leave the poor hapless receptionist hanging out to dry if the hospital caught major heat for such bold actions.
To tell the truth, in the subsequent 30 years I’ve practiced medicine, this type of person with this type of ethical and moral strength seems to have died out. This type of safeguard depended upon honor, integrity and – yes, morals. Today’s litigation and liability climate seems to have made such procedures extinct.
**********
**********
4. When the preliminary results from the blood substitute study were published in Jan. 2009, they were hard to interpret. The article seems to say that patients who were given Polyheme ended up about the same as those who didn’t get Polyheme – but since the Polyheme didn’t complicate things, then it was promising.
In fact, the company later asked an outside company to review the records and see if there was any difference between the two groups of patients. If they had asked me (who would be so foolish?) I would have noted the obvious fact that there were three times as many folks who died of heart attack in the group with the Polyheme as in the other group (3% vs. 1%).
When I was conducting clinical trials as a primary investigator, I have been asked to stop work with experimental protocols (commercial drug companies for anti-anxiety and anti-depressant drugs) for less impressive statistics of danger from the drug being studied.
In my personal analysis, there is also nothing I can see from this article that looks anything like a real advantage to using Polyheme. They have chosen as the endpoint for this study “a dual superiority/non-inferiority endpoint.” In plain English, that means that Polyheme is at least as good as salt water and it doesn’t seem to be any worse than salt water.
Is this what you want to prove in a study of folks with life threatening conditions? Can’t more be done with the data?
5. Any clinical trial must strive to be as ethical as possible. There are a lot of people in this story who are not identified. The single most important group, the one that is pledged to be a “safeguard” in this sort of abuse, is the IRBs. By federal law, there has to be not one but several IRBs or “Institutional Review Boards.” At least 29, since it says 29 trauma centers were involved.
Most trauma centers have a University affiliation, and Universities usually require that their professorial medical staff — and at least one would have to take responsibility for this — review the protocol.
Folks try to be ethical, I know, but I have personally dealt with not one, but two University-based Institutional Review Boards where people told me (without witnesses) that they found it “easier” to pass protocols to study commercial drugs because they “knew” they had already been passed by other review boards. You understand – it must be okay because everybody else is doing it.
In case you weren’t aware of how this type of research works, these trauma centers are making a LOT of money and are paid a huge fee per patient enrolled in this study. You better believe this is an incentive to actively recruit patients. Most universities and many hospitals count on these fees for a large part of their budget.
The kind of severe trauma we are talking about in the case of Polyheme is most common in folks from the lower socio-economic classes. So what gives these people an incentive to volunteer for something that might be risky? They are compensated – sometimes handsomely – for simply showing up and allowing the researchers to carry out the tests. In my experience doing clinical trials both in university settings and in my own private research institutions, I’m familiar with the type who are willing to take risks to collect personal compensation in clinical trials. This is a recognized phenomenon called “Guinea Pigging” and was the subject of an article in The New Yorker a couple of years ago.
I won’t go so far as to say that in some institutions, these folks are often undervalued as human beings, but the financial gains of conducting a clinical trial on this level is great. Giving a few bucks to the needy for the use of their bodies seems like a cheap way to keep the money rolling in.
The ironic thing is that — in the case of Polyheme — the “recruits” were unconscious and didn’t volunteer for the test, and they weren’t given any financial compensation. I suppose they should be grateful if the treatment spared their lives.
Also, there is a budget item called “indirect costs” — meaning overhead. An institution of higher education that teaches medicine can make a LOT of money — sometimes well over 50% of money paid by the drug or substance developer – by charging indirect costs. These funds are used to pay the supervising professor, the lower level workers who do most of the work of administering the protocol — which is often minimal, and compensate the institution for the usage of rooms, heating and air conditioning, lights, security, parking – whatever else is included in “overhead”.
6. As I mentioned at the beginning, the people at Northfield Laboratories who — if not originated — at least were trying to exploit this substance, bet the farm and lost. The FDA shut them down — appropriately but late, I believe — on May 9, 2009. Their verdict – the risks outweighed the benefits. The comparison to salt water must have been overly-optimistic. The company reportedly lost $220 million on Polyheme and declared bankruptcy June 1, 2009.
On the company website, Northfield tried to justify its actions:
- It listed the FDA rules for a waiver of informed consent under certain conditions. Whether Polyheme fell under those rules wasn’t discussed.
- The protocol was passed by the FDA and approved by 32 IRBs.
- “Community consultations” were conducted by participating institutions, including public meetings, print and broadcast “media impressions.”
- An Independent Data Monitoring Committee reviewed data periodically and recommended continuing the study after each review.
- “Patient enrollment” – of unconscious people – surpassed the 700 mark. (As if the patients made a voluntary choice)
I won’t condescend to pointing out how self-serving these statements can be, and how little they actually mean in justifying the Polyheme trials.
As far as I can tell, Northfield never made their protocol – the rules by which testing was conducted — public. I can understand them claiming that things are proprietary at this point is an attempt at self-defense. In fact, they sued the San Diego Reader (who wrote an excellent expose’) to keep that publication from printing what the company termed “trade secrets.” I would be quite surprised if there were not numerous people lined up wanting to sue this company for wrongful death of a loved one. I don’t know what made 3% of participants have heart attacks. Despite their outside review, I don’t think they do either.
7.There were some major faults in the writing of this protocol, as far as I can tell from the little information I have about it. My understanding, from the few cancer chemotherapy-type protocols I have seen, is that you offer someone an experimental treatment when you can be reasonably assured, in a life-threatening case, that the chance of sustaining life is increased with the experimental treatment. Were patients who might have been better off with standard treatment denied that very treatment so that Ployheme could be given a try?
The average human red blood cell, which is being used as the medium of oxygen transport in transfused blood, lives 120 days. The phase III, or study to look at clinical utility beyond the one cited in the published literature, takes as its endpoint 30 days of survival of the patient. Now we are not given the time of viability of Polyheme; that is, we have no idea how long it works until it needs to be replaced, but I would bet it is less than 120 days. That means that, possibly, an argument could be made for trying Polyheme in the field. There are no other options available, blood typing takes time and is not generally done in the field. Maybe there is nothing else here and it is worth a trial.
But patients in the field are usually taken to the hospital fairly quickly, and usually to a trauma center, which would be very capable of matching and transfusing blood. Since the latter treatment has been, for whatever reason, the standard of care, it is frankly unethical to deprive the patient of this standard of care in favor of a product that can only last less long than a transfused blood product.
McGill Journal of Medicine reviews, in excellent clinical context, the disaster of Polyheme
8. To me there is one part of this tragedy that is more outrageous than the rest. One of the regional primary investigators is in my hometown at the University of San Diego School of Medicine. His efforts to go forward with this trial appear to lack ethical or moral context. I have never met Dr. Dan Davis, the local primary investigator. However, as an ex-academic, I am aware of the pressure that a medical school can put on someone in his position if it means $2.3 million from the National Institutes of Health. Certainly the uinversity’s bean-counters would be willing to accept the fact that “other risks should be minimized” because there was no possible informed consent for this clinical trial.
The monetary windfall may also have had something to do with the initially apparent complicity of the city and its emergency services in this debacle. It is logical that the University “recruited” the city’s EMS with substantial cash to administer the Polyheme instead of salt water to unconscious victims and to record the results. Ultimately, EMS bowed out. They made this decision secretly, so even excited medicine watchers such as myself had no real idea what was going on.
It must have been something scary for our financially strapped city to bow out of something where big money must have been involved.
In the morass of publicity that could have followed, it seems as if a lot of people were worried about negative reactions to the trial. But one of the things that needed to happen was that the people who lived in the parts of the city that would be involved (the areas where the most emergency calls are responding due to various factors) in the trial be notified. This might have reduced the risk of the questionable use of the impossible informed consent.
This absolutely did not happen. Remember the list on the company website about “community consultations?” These efforts to inform the public resulted in a single public meeting led by Dr. Davis where three people were present; two reporters and one friend of the reporter who wrote this up for the San Diego Reader. This effort at public awareness was the responsibility of Dr. Davis, as it would have been the responsibility for the local primary investigator of any multi-center clinical trial. The efforts were – let’s just say “inadequate.”. Remember the company’s claim about “media impressions?” Locally, they said it could not be done, there was not enough money for television commercials.
These protests all ring hollow. If you value such ideals as informed consent, you find a way. There is a great deal known about the people who get into clinical trials, even if not specifically this kind of clinical trial. They are, by and large, poor and disenfranchised folks. They do not come to meetings at libraries. They talk to people from their own community whom they trust. They are more likely to respond to handbills in the street than to a library talk. Some may even respond to a website.
Even if he or she does not know how to reach those potentially affected, a reasonable local primary investigator needs to make sure his clinical trial is ethical. Those who do not know ask for help.
Again, I don’t know Dr. Davis. Perhaps he wasn’t experienced as a Primary Investigator and hadn’t had experience in these matters. However, if he was in charge of a major project at a major University, one would think he had the experience and the resources.
I have agonized — yes, agonized — as a primary investigator in multi-center commercial trials of drugs that would be considered benign in comparison to Polyheme, about doing the right thing for my patients. About making very sure that I value their lives first. The Hippocratic Oath. That is still the spirit, at least, of what it means to be a doctor.
The company, the university, the primary investigator, even the city of San Diego seem to hide from blame with a smokescreen of excuses and justifications – when it all boils down to: The money was too good to refuse, no matter what the risks.
What needs to happen at this level — as well as at all levels reviewed above — is some consideration of basic, human commonsense ethics. If people cannot give informed consent, somebody has to take responsibility for the patient being “correct” for the clinical trial. All sources listed above have “protocol violations” so it sounds as if even another level, the enrollment of people in the protocol may have been done gratuitously. Again — this means extra revenues.
But back to basic, human commonsense ethics, which have completely disappeared.
1.The first thing we need is something to happen with the Investigational Review Boards to make sure we are not looking at rubber stamping of protocols. I have long wondered about who these kinds of boards really work for. Maybe a truly “independent” one is needed, instead of one housed in and comprised of the University and its crowd.
2. The idea of the Polyheme kind of molecule is nice, even elegant. It is common for clinical testing to begin with lab animals. Are people scared of People for the Ethical Treatment of Animals or does the extra step get in the way of “fast track” quick approval – and quicker profits? I do not know if the company went through traditional animal testing, but it could have saved a couple of lives.
3. I am certain that the system can somehow work with an institutional surrogate informed consent. I know I’ve seen the need for it in my previous life as a surgeon. It has a place in medicine and can mean life instead of death in certain situations. However, we need to question the propriety of using such a delicate decision simply to increase enrollment into a for-profit clinical trial. At risk of repeating myself, there is a human life involved and the patient is giving the doctor or hospital a sacred trust – even if involuntarily – to do the very best thing possible in the best interest of the patient. That is what ethics is about – not self-interest for the financial solvency of a department, institution or regulatory entity. Be it a technician or administrator, there should be someone who has no financial interest in the protocol. I am an expert in this because back when I was a lowly receptionist I phoned people like this at home and reported cases. They were responsible, caring, and asked the right questions.
4. Review of preliminary study results can give big hints if the product is a “dud.” As mentioned above, Northfield reviewed data (they say) at various points in the trial.
“An Independent Data Monitoring Committee is charged with overseeing patient safety in this study. After reviewing the data on the first 60, 120, 250, and 500 of the planned 720 patients to be enrolled in the study, the IDMC four times recommended that the study continue without modification. Following the 500 patient review, the IDMC recommended that the study go to completion.”
If no data shows that the study is giving results at least as good or better than the existing treatments, somebody needs to call a halt.
Sure, drugs that are not pulled immediately may be pulled later. Sure, money has already been put in and people do not want to pull out, but lives have been put in, too. Let’s look at least at how many lives have been lost with study substance.
5. Acknowledge the amount of money that the drug company pays to a person or institution and make it part of the informed consent. People make financial disclosures in far less important places. The human subject deserves to know.
6. Anything that could be killing people should not be tested further. Is 3% an acceptable loss, and if so – under what circumstances? I don’t care what impartial observers say. This was time to pull the substance.
7. The protocol does not seem to me to have been intelligently and ethically written. I do not have all of the information about this, but it seems to me totally unethical that the Phase III includes both a pre-hospital and in-hospital section, when currently existing mechanisms for transfusion are available after arrival at the hospital. If this stuff needs testing at all, limit to pre-hospital phase, please. N.B. previously cited article from McGill Medical Journal speaking of clinical testing of blood-like products says exactly the same thing as me.
8. What is a clinical investigator? What is a doctor? It is someone for whom the “buck stops here” on science and ethics — Somebody who knows how to administer a clinical trial as well as how to take care of patients.
People asked me all the time when I was in the middle of a research protocol whether I was a researcher first or a doctor first. I told them then and tell everyone now that I am a doctor first. If a patient can be treated better without a clinical trial, I have always pulled them off the clinical trial and gotten them to the best treatment. Always.
As I mentioned, it is possible that Dr. Davis was inexperienced as an investigator or perhaps the University has pushed him into earning his own salary from drug companies. But the primary duty of a medical doctor should be to think about what he is doing and what his responsibilities are – not how to generate funds for the institution.
Obviously, I am nothing short of delighted that the FDA has pulled Polyheme. This program was totally devoid of ethics.
There may be little or no advancement in medicine in the future. The system of pharmaceutical industry sponsored clinical trials, and perhaps all clinical trials, has long ceased to reflect the higher ethics, the freedom of thought, which may have been part of the University system during the middle ages.
Now, the few sincere academic researchers left are retiring and dying. The main reason I left academics was because of the way research was being conducted. I went and started my own research institution — and lost money by doing it ethically. Ethical research in academic and public settings has been replaced with research that is profit-motivated and has no reasonable consideration for humans. There is no bioethics.
The depths of my sadness are great.
Filed under Research by admin on Feb 24th, 2010. ![]()
Leave a Comment